Case Report
Nutcracker Syndrome: A Case Report of Renal Vein Compression between the Aorta and Vertebra
- Layth Al-Karaja
Corresponding author: Layth Al-Karaja, Faculty of Medicine, Al-Quds University, Jerusalem, Palestine.
Volume: 2
Issue: 4
Article Information
Article Type : Case Report
Citation : Obayda M. Nafaa, Shifaa Mustafa, Alaa Hmeedan, Eman Jamal Shawahna, Abed Saleh Hassouna, Laith B. Nassar, Diya Asad, Layth Al-Karaja. Nutcracker Syndrome: A Case Report of Renal Vein Compression between the Aorta and Vertebra. Journal of Medical and Clinical Case Reports 2(4). https://doi.org/10.61615/JMCCR/2025/AUG027140829
Copyright: © 2025 Layth Al-Karaja. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.61615/JMCCR/2025/AUG027140829
Publication History
Received Date
13 Aug ,2025
Accepted Date
25 Aug ,2025
Published Date
29 Aug ,2025
Abstract
Nutcracker syndrome (NCS) is a rare vascular disorder characterized by compression of the left renal vein between the abdominal aorta and the superior mesenteric artery (SMA), leading to a spectrum of symptoms including hematuria, flank pain, and varicocele. We present a unique case of NCS in a 35-year-old female who presented with persistent left flank pain and hematuria. Further imaging revealed compression of the left renal vein between the abdominal aorta and the adjacent vertebral body, an exceedingly rare variant of NCS. The patient was managed conservatively with close follow-up, and his symptoms improved over time. This case highlights the importance of considering atypical anatomical variations in the diagnosis and management of NCS.
Keywords: Nutcracker syndrome (NCS), left renal vein (LRV), vascular compression, hematuria, posterior nutcracker syndrome (PNCS)
►Nutcracker Syndrome: A Case Report of Renal Vein Compression between the Aorta and Vertebra
Obayda M. Nafaa1, Shifaa Mustafa2, Alaa Hmeedan3, Eman Jamal Shawahna4, Abed Saleh Hassouna5, Laith B. Nassar5, Diya Asad6, Layth Al-Karaja6*
1Jenin-Government Hospital, Jenin, Palestine.
2Pediatric Department, Specialized Arab Hospital, Nablus, Palestine.
3Internal Medicine Department, An-Najah National University, Nablus, Palestine.
4Faculty of Medicine, An-Najah National University, Nablus, Palestine.
5Rafidia Surgical Hospital, Nablus, Palestine.
6Faculty of Medicine, Al-Quds University, Jerusalem, Palestine.
Introduction
Nutcracker Syndrome (NCS) is the fancy term used to describe the compression of the left renal vein (LRV) and can be congenital or acquired. There are two types: Anterior Nutcracker Syndrome, the better-known variant, in which the left renal vein is compressed between the abdominal aorta and the anterior mesenteric artery due to congenital or acquired reduction in the aorto-mesenteric space through which the left renal vein passes, and Posterior Nutcracker Syndrome, the less common variant, describes the state of the left renal vein being compressed between the abdominal aorta and the lumbar vertebral body.[1]
Posterior Nutcracker syndrome (PNCS) is caused by underlying anatomical anomalies such as the Retroaortic renal vein (reported incidence is 1-2.4%) and renal collar. Contributing factors have been suggested, such as ptosis of the left kidney with the subsequent stretching of the vein, the presence of an abdominal aortic aneurysm, lumbar vertebral osteophytosis, or pregnancy, but these factors are absent in most patients. [2-4]
PNCS is most commonly a phenomenon manifested only on imaging without clinical manifestations. When symptomatic, it can manifest clinically with intermittent microscopic or gross hematuria, flank pain of varying severity, gonadal or spermatic reflux, and pelvic varices. [5,6]
Diagnosis of PNCS is usually delayed and overlooked, especially when only routine diagnostic procedures are used. Doppler ultrasonography is the first line of imaging, and contrast-enhanced computed tomography scans provide more accurate vascular diagnosis and help exclude other potential causes of trapping.[6] Management of posterior Nutcracker syndrome has both conservative and invasive approaches; the decision depends on the age, the severity of the symptoms, and comorbid or contributing factors.[7]
Herein, we present the case of a thirty-five-year-old female patient with known single left kidney and unremarkable medical history who was ultimately found to have posterior nutcracker syndrome on contrast-enhanced computed tomography after complaining of left flank pain and occasional episodes of gross hematuria for ( I don’t know this detail), To our knowledge, this is the first case of PNCS in a young female with single left kidney, complicating the situation and limiting the possible management options. Our patient was successfully managed conservatively.
Case Presentation
A thirty-five-year-old female patient who is known to have a single functioning left kidney due to a congenitally atrophied right kidney on regular follow-up was in her usual state of health until 2016, when she started to complain of recurrent episodes of left flank pain and hematuria. The patient was treated with painkillers and antibiotics with no improvement. However, her symptoms persist. A cystoscopy to rule out malignancy or urinary tract lesions was performed, during which a tissue biopsy was done. No lesions were identified, and the histopathology result came back normal. Her laboratory investigations, including kidney function test, complete blood count, and full chemistry panel, were all within normal limits. Shown in tables (1-3). Urine analysis revealed microscopic hematuria, and an ultrasound was done and resulting in an atrophied right kidney and hypertrophic left kidney.
|
Test |
Result |
Normal range |
|
Hemoglobin |
14.5 |
12-16 |
|
White blood cells |
5.8 |
4.6-11 |
|
Platelet count |
245 |
150-450 |
Table 1. Complete Blood Count
|
Test |
Result |
Normal range |
|
Specific gravity |
1.020 |
1.003-1.029 |
|
PH urine |
6 |
4.5-7.8 |
|
Protein |
Trace |
- |
|
Glucose |
- |
- |
|
Ketones |
- |
- |
|
Bilirubin |
- |
- |
|
Blood |
++ |
- |
|
Leukocytes |
- |
- |
|
Nitrite |
- |
- |
|
Urobilinogen |
Normal |
0.1-1 |
|
WBCs |
1-3 |
0-5 |
|
RBCs |
30-35 |
0-5 |
|
Epithelial cell |
+ |
0-10 |
|
Mucus |
+ |
- |
Table 2. Urine Analysis
|
Test |
Result |
Normal range |
|
Creatinine |
0.72 |
0.5-0.9 |
|
Albumin |
4.80 |
- |
|
Potassium |
4.2 |
3.5-5.3 |
|
Sodium |
143 |
135-145 |
Table 3. Serum Chemistry
Later on, the patient continued to complain of flank pain and gross hematuria, so that a renal Computed Tomography scan with and without intravenous contrast was performed, which showed that the left kidney was hypertrophied, measuring about 13 cm in its bipolar length. Otherwise, normal in shape and position with no definite lesions or hydronephrosis, normal excretion, the right kidney is atrophic, with no hydronephrosis. The left renal vein is compressed between the aorta and vertebral body with dilation proximal to the stenosis. Figure 1
Figure 1, Part A; Axial CT scan, delayed phase: mild free fluid.
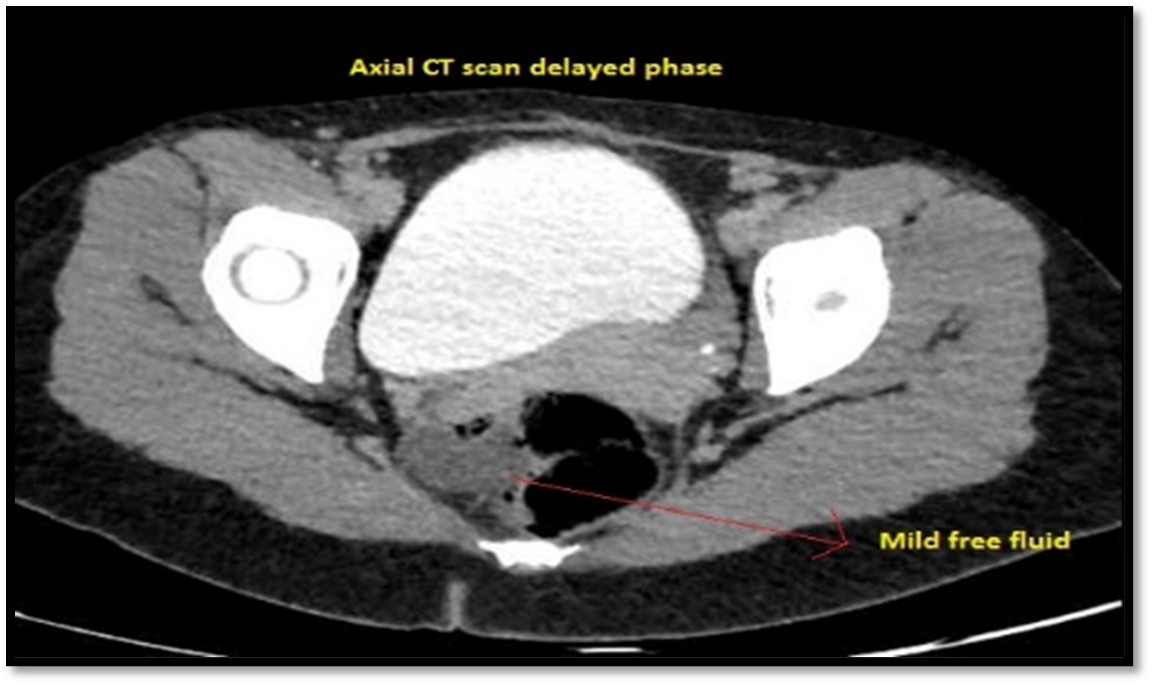
Figure 1, Part B; Coronal CT scan without contrast: atrophied right kidney & hypertrophied left kidney.
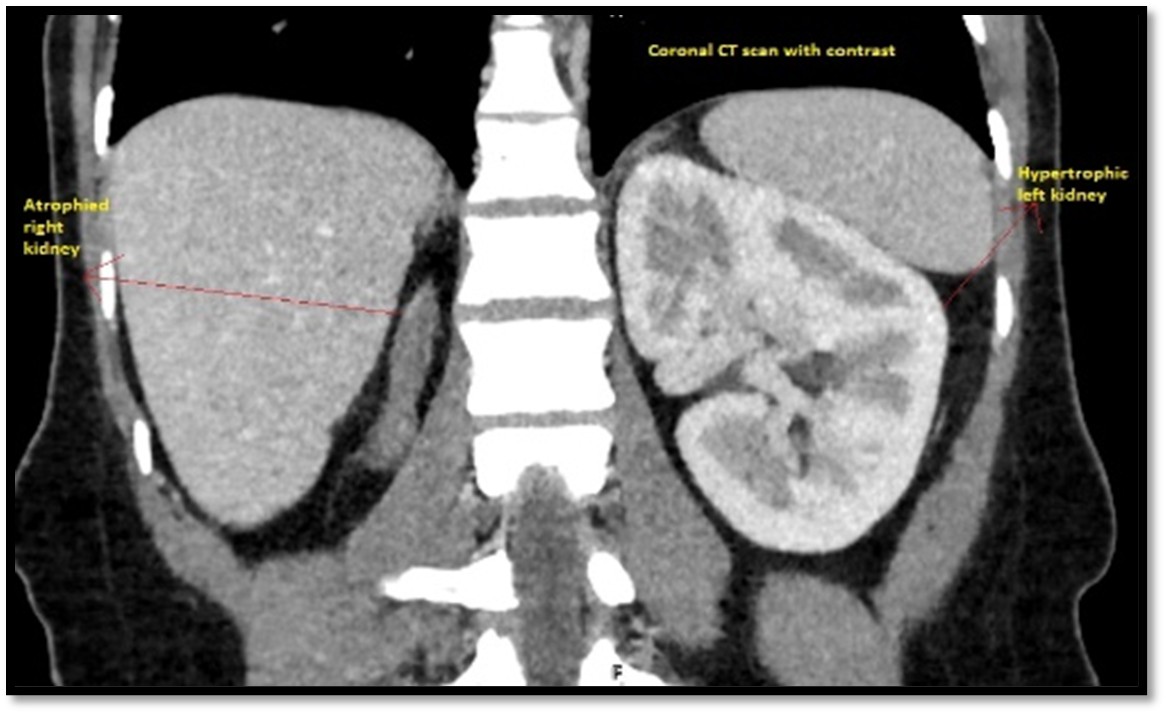
Figure 1, Part C; Axial CT scan: left renal vein compressed between aorta and vertebra.

Figure 1, Part D; Coronal CT with contrast: bulky uterus with congested para-uterine arteries.

The treatment plan for the patient was discussed with the vascular surgery team for renal vein stenting, or bypass, and possible renal transplantation if other measures had failed, taking into consideration the fact that our patient has a single-functioning kidney, further complicating the management decision.
Discussion
Posterior Nutcracker Syndrome is a rare yet potentially serious condition. Posterior nutcracker syndrome occurs when the left renal vein becomes compressed between the aorta and the superior mesenteric artery. This compression leads to venous congestion and hypertension in the left kidney, ultimately posing a risk of kidney damage. The estimated prevalence of this condition in the general population ranges from 0.1% to 3.0%.[8]
The exact pathogenesis of retroaortic left renal vein (LSRV) compression syndrome remains incompletely understood. It is believed to arise from congenital anatomical variations in the relationship between the aorta and the LSRV. Typically, the LSRV courses anteriorly to the aorta. However, in patients with retroaortic LSRV compression syndrome, the LSRV takes a posterior route behind the aorta. This abnormal anatomical configuration results in compression of the LSRV between the aorta and the vertebral column. [9,10]
Clinical presentation varies based on the degree of compression. Patients may exhibit symptoms such as abdominal pain, flank pain, hematuria, and proteinuria. In severe cases, renal insufficiency or even renal failure can ensue. [11,12]
Diagnosis relies on clinical findings and imaging studies. Duplex ultrasound allows visualization of the LSRV and assessment for compression. Magnetic resonance imaging (MRI) and computed tomography (CT) are additional modalities used to confirm the diagnosis.[13]
The prognosis for patients with nutcracker syndrome is not well confirmed, but it is generally favorable with endovascular intervention for anterior nutcracker syndrome, and a left renal vein transposition in open surgery for posterior nutcracker syndrome, as most individuals experience significant symptom improvement following these two interventions, according to the type of the syndrome. [14,15]
Case Reports and Considerations in Retroaortic LSRV Compression Syndrome: In the medical literature, several case reports shed light on retroaortic left renal vein (LSRV) compression syndrome.
A 5-year-old boy presented with a 2-year history of intermittent hematuria, worsening to daily episodes in the preceding 6 months, especially following physical exertion. Abdominal and pelvic CT imaging revealed retroaortic compression of the left renal vein by the aorta, consistent with posterior nutcracker syndrome (PNS).[16]
Another case report of a 62-year-old Caucasian male who presented to a radiology department for chronic hepatitis B-related liver disease follow-up and complained of mild scrotal pain. Ultrasound revealed compression of the left retro-aortic renal vein within the aorto-vertebral space, attributed to an osteophyte.[17]
These case reports underscore the importance of considering retroaortic LSRV compression syndrome in patients presenting with unexplained flank pain, hematuria, proteinuria, or scrotal pain. Early recognition and timely intervention are crucial to prevent serious complications.
In the current case, the patient presents with a unique twist: posterior nutcracker syndrome and a solitary functioning kidney. This poses a challenge for treatment planning, as any intervention carries heightened risks compared to a typical posterior nutcracker syndrome scenario.
A report presents two cases of posterior nutcracker syndrome (PNS) successfully treated with a novel self-expanding venous stent, representing the first reported use of this device for complete endovascular PNS management. While clinically indistinguishable from anterior nutcracker syndrome (NS), subtle technical differences exist, necessitating indirect assessment of compression when intravascular ultrasound is unavailable. Although the renocaval gradient applicability remains unclear for PNS, their medium-term follow-up demonstrates comparable safety and efficacy of endovascular treatment for both PNS and NS, suggesting this approach is a viable and effective option for PNS.[18]
In another case of posterior nutcracker syndrome, left renal vein (LRV) anterior transposition proved a safe and effective technique, offering a tension-free repair without prosthetic material and eliminating potential thromboembolic risks associated with incomplete LRV detachment. While this approach necessitated clamping of the common iliac veins and inferior vena cava, introducing risks of clamp injury and bleeding, the overall outcome supports its consideration as a viable treatment option for PNS.[19]
In the context of this patient, a multidisciplinary approach is needed to plan the management of the patient, as crafting an optimal treatment plan necessitates individualization. Each treatment option must be meticulously evaluated, weighing its associated risks and benefits before arriving at a decision.
Compared to previously documented cases, the present situation stands out due to the patient's singular functioning kidney. This uniqueness amplifies the complexity of treatment planning, as any intervention inherently carries heightened risks of mortality and morbidity when contrasted with a typical posterior nutcracker syndrome scenario.
Indeed, the current case diverges from the earlier literature reviews. The patient's sole functioning kidney further complicates the treatment landscape, demanding thoughtful consideration and tailored management strategies.
Conclusion
In conclusion, we presented a rare case of nutcracker syndrome (NCS) in which the left renal vein was compressed between the abdominal aorta and an adjacent vertebral body. Despite its rarity, this case underscores the importance of considering atypical anatomical variations in the diagnosis and management of NCS. Awareness of such variations is crucial for accurate diagnosis and appropriate management of patients presenting with symptoms suggestive of NCS. Further studies are warranted to better understand the clinical significance and optimal management of this rare variant of NCS.
Data Availability
This published article comprises all data generated or analyzed in the context of this case.
Ethical Consideration
Our institution does not require ethical approval to report individual cases or case series.
Consent to Participate
Written and oral informed consent was given by the patient.
Consent for Publication
Written informed consent was obtained from the patient for their anonymized information to be published in this article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Funding Statement
This study received no funding.
- Yun SJ, Lee JM, Nam DH. (2016). Discriminating renal nutcracker syndrome from asymptomatic nutcracker phenomenon using multidetector computed tomography. AbdomRadiol (NY). 41(8): 1580–1588.
- Singla RK, Sharma T, Gupta R. (2010). Retro-aortic left renal vein with left suprarenal vein draining into inferior vena cava. Int J AnatVar. 3:134–137.
- Rassi I, Khabbaz Z, Chelala D. (2010). A new variant of the posterior nutcracker phenomenon. J VascSurg. 51(5): 1279.
- Puig S, Stühlinger HG, Domanovits H. (2002). Posterior “Nutcracker” phenomenon in a patient with abdominal aortic aneurysm. EurRadiol. 12(3): 133–135.
- Lamba R, Tanner D, Sekhon S. (2014). Multidetector CT of vascular compression syndromes in the abdomen and pelvis. Radiographics. 34(1): 93–115.
- Gozzo C, Giambelluca D, Cannella R. (2020). CT imaging findings of abdominopelvic vascular compression syndromes: what the radiologist needs to know. Insights Imaging. 11(1): 48.
- Marone EM, Psacharopulo D, Kahlberg A. (2011). Surgical treatment of posterior nutcracker syndrome. J VascSurg. 54(3): 844–847.
- Praveen M, Suseelamma D, Saritha S. (2012). Multiple renal vascular variations. Open Access Sci Rep. 1(6):334.
- Yun SJ, Lee JM, Nam DH. (2016). Discriminating renal nutcracker syndrome from asymptomatic nutcracker phenomenon using multidetector computed tomography. AbdomRadiol (NY). 41(8): 1580–1588.
- Butros SR, Liu R, Oliveira GR. (2013). Venous compression syndromes: clinical features, imaging findings and management. Br J Radiol. 86(1030): 20130284.
- Gozzo C, Farina R, Foti PV. (2021). Posterior nutcracker syndrome: a case report. J Med Case Rep. 15(1): 42.
- Ananthan K, Onida S, Davies AH. (2017). Nutcracker syndrome: an update on current diagnostic criteria and management guidelines. Eur J Vasc Endovasc Surg. 53(6): 886-894.
- He Y, Wu Z, Chen S. (2014). Nutcracker syndrome--how well do we know it? Urology. 83(1): 12-17.
- R. Chiesa, A. Anzuini, E.M. Marone. (2001). Endovascular stenting for the nutcracker phenomenon. J Endovasc Ther. 8(6): 652-655.
- B. Ali-El-Dein, Y. Osman, A.B. Shehab El-Din. (2003). Anterior and posterior nutcracker syndrome: a report on 11 cases Transplant Proc. 35(2): 851-853.
- Parulkar BG, Kulkarni P, Chandrasekhar R. (2002). Retroaortic left renal vein entrapment: a laparoscopic approach. Surg Laparosc Endosc Percutan Tech. 12(5): 344-346.
- Gozzo C, Farina R, Foti PV. (2021). Posterior nutcracker syndrome: a case report. J Med Case Rep. 15(1): 42.
- Rodríguez-Morata, Alejandro. Endovascular treatment of posterior nutcracker syndrome with a new autoexpandable stent. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 7(1): 118–121.
- Moreira MC, Amato MB, Costa-Pereira AP. (2011). Endovascular treatment of nutcracker syndrome with venous stents. J Vasc Interv Radiol. 22(11): 1618-1623.
Download Provisional PDF Here
PDF




p (1).png)




.png)




.png)
