Case Report
Acute Appendicitis in a 103 Years Old Male Patient: Uncommon Age for a Common Disease, A Case Report and Review of Literature
- Ahmad Reza Shahraki
Corresponding author: Ahmad Reza Shahraki, General Surgeon, Assistant Professor, Department of Surgery, Medical Faculty, Zahedan University of Medical Sciences and Health Services, Zahedan, Iran. Orcid Id: https://orcid.org/my-orcid?orcid=0000-0002-9288-977X
Volume: 2
Issue: 6
Article Information
Article Type : Case Report
Citation : Ahmad Reza Shahraki. Acute Appendicitis in a 103 Years Old Male Patient: Uncommon Age for a Common Disease, A Case Report and Review of Literature. Journal of Medical and Clinical Case Reports 2(6). https://doi.org/10.61615/JMCCR/2025/DEC027141205
Copyright: © 2025 Ahmad Reza Shahraki. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.61615/JMCCR/2025/DEC027141205
Publication History
Received Date
19 Nov ,2025
Accepted Date
02 Dec ,2025
Published Date
05 Dec ,2025
Abstract
This case report has been reported in line with the SCARE Criteria. Acute appendicitis is a common acute surgical abdominal condition, and despite the majority of cases being observed in children and young adults, its occurrence in the elderly seems to be increasing, with a higher risk of perforation. With increased life expectancy and the growing total population of elderly patients, there has been a rise in the number of cases of acute appendicitis in elderly people. Although acute appendicitis is not the most typical pathological condition in the elderly, it is not uncommon. Most of these patients require surgical treatment, and as with any acute surgical pathology in advanced age, treatment possibilities are affected by comorbidities, overall health status, and an increased risk of complications.
This case is about a 103-year-old male with abdominal pain and Acute appendicitis, that which CT shows inflammation and appendectomy in safe mode did and he was discharged healthy.
Appendicitis, an inflammation of the vermiform appendix, is one of the most common causes of acute abdomen and one of the most frequent indications for emergency abdominal surgery worldwide. Any person older than 65 years old is considered elderly. The elderly population constitutes only 5-10% of total appendicitis cases. The symptoms depend on the location of the appendix. Generally, lower abdominal pain and anorexia are known to be the most common symptoms of appendicitis. Although young adults have a higher prevalence of appendicitis, the elderly have a higher complication rate, 37.5% versus 43.97%. Acute appendicitis in the elderly constitutes a small percentage of total appendicitis cases, has a wide range of presentations, and is associated with a higher rate of complications, making it a challenging diagnosis. Thus, we believe that acute appendicitis in the elderly needs to be further studied, and more data should be added to the literature, which will help establish the diagnosis of appendicitis to avoid delayed diagnosis and possible complications. Findings suggest an increased risk of peri-and postoperative complications among elderly subjects undergoing appendectomy, compared to non-elderly subjects.
Key words: typical appendicitis in the elderly, simple appendicitis, appendicitis in the elderly, acute appendicitis elderly, acute appendicitis, surgery.
►Acute Appendicitis in a 103 Years Old Male Patient: Uncommon Age for a Common Disease, A Case Report and Review of Literature
Ahmad Reza Shahraki1*
1General Surgeon, Assistant Professor, Department of Surgery, Medical Faculty, Zahedan University of Medical Sciences and Health Services, Zahedan, Iran.
Introduction
Appendicitis is an inflammation of the vermiform appendix. It is one of the most common causes of acute abdomen and one of the most frequent indications for emergency abdominal surgeries worldwide (1). In clinical practice, treating patients based on their age group is one of the important considerations clinicians should keep in mind. It is important to identify a patient’s age group to foresee how they may differ from the typical disease presentation. Elderly people are defined as any person aged 65 years or older (2). Appendicitis in elderly patients accounts for 5-10% of total cases (3). The prevalence of complicated appendicitis increases with age, reaching 37.5% in patients aged 40-64, 43.97% in those aged 65-74, and further rising to 56.84-63.0% for patients aged above 75 and 64.9-72.7% for those over 80 years old (4,5). Acute appendicitis is one of the most common surgical pathological conditions, with a lifetime risk of 7–8% (35). In the Western world, the incidence of acute appendicitis has been stable over the last 20 years after a decrease in the 20th century, but recently there has been an increase in incidence in South America, Asia, and the Middle East (36,37,38). The incidence of acute appendicitis in the elderly is rising due to a longer life expectancy (37). The most common symptoms associated with acute appendicitis are also observed in elderly patients—lower abdominal pain (93.9–97.6%), anorexia (57.6–67.0%), nausea and vomiting (45.5–68.3%), shifting pain (30.3–45.1%), right iliac fossa pain (60.6%), and pyrexia (21.2–26.8%) (39, 40). Elderly patients may not have conclusive clinical signs of acute appendicitis, but signs of peritonitis—abdominal distention, reduced abdominal wall movement, severe tenderness, localized and generalized guarding—are more pronounced (38).
Case Presentation
This case is about a 103-year-old male with abdominal pain for 2 days before, and no recurrent similar pain before that, admitted to the general surgery part. Examination started, and the lab data were normal, and in his body just we found RLQ tenderness. CT was done and just shows inflammation in the fat around the appendix. We decided to perform a surgery in the midline parts, and in the surgery, we found acute appendicitis (Figure 1) with normal small and large bowel. One day after surgery, we started eating, and we discharged him 2 days after admission, healthy.

Figure 1: Acute Appendicitis.
Discussion
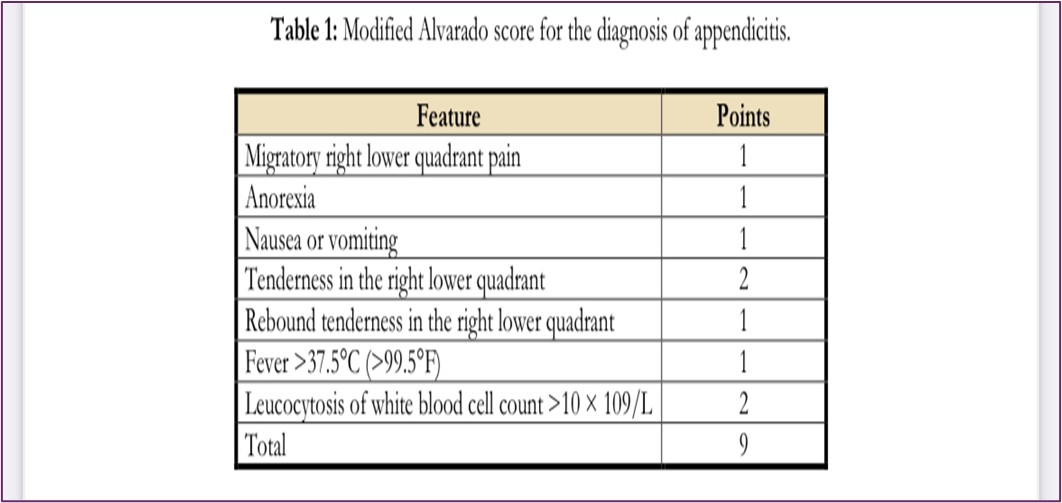
Acute appendicitis is mainly caused by a luminal obstruction that can lead to inflammation, ischemia, and, consequently, perforation and peritonitis or a contained abscess. The cause of obstruction differs according to age. At a young age, lymphoid follicular hyperplasia is the most common cause of obstruction of the vermiform appendix, whereas in older adults, fecolith, fibrosis, and neoplasia are the most common causes. When obstruction occurs, the intraluminal and intramural pressure of the appendix increases, leading to the occlusion of small vessels and resulting in ischemia (4). Multiple risk factors for appendicitis have been reported in the literature, including unhealthy diet, smoking, a family history of appendicitis, low socioeconomic status, and the use of probiotics and antibiotics (7). The typical symptoms of acute appendicitis include colicky pain that starts in the periumbilical area and then becomes constant and sharp, ultimately shifting to the right lower quadrant with tenderness at McBurney’s point. Anorexia, nausea, vomiting, and fever are associated symptoms (8). The accuracy of the diagnostic evaluation relies on the experience of the attending physician. A high index of suspicion is crucial as elderly patients can present with atypical symptoms. A combination of clinical signs, laboratory findings, and imaging is important to establish a diagnosis. The laboratory tests for suspected acute appendicitis should include a complete blood count with differential and serum C-reactive protein, with their combination significantly increasing the sensitivity. Although there are many scoring systems for the diagnosis of acute appendicitis, the most common is the modified Alvarado score (Table 1). A score of ≤3 suggests that the diagnosis of appendicitis is unlikely and another diagnosis should be considered, while patients with a score of >3 should undergo further evaluation for appendicitis (9). The definition of the term “elderly” is somewhat unclear. Conventionally, it has been considered a chronological age of 65 or older, but the World Health Organization and the Japanese Geriatrics Society have recently suggested a cut-off value of 75 or older based on improvements in physical function over the last 10–20 years (23).
Contrast-enhanced CT of the abdomen is the imaging modality of choice, while ultrasound and magnetic resonance imaging are reserved for children and pregnant women. The findings on CT can include appendiceal wall thickening or enhancement, peri-appendiceal fat stranding, and/or appendicolith (10). The standard management of acute appendicitis is an appendectomy, either a laparoscopic or an open appendectomy. Recent studies suggest that conservative management with antibiotics is not inferior to surgical management in many cases (11). However, for elderly patients in particular, a small study reported a 20% recurrence rate for those who were managed conservatively (12). In elderly patients with appendicitis, the diagnosis may be challenging as the classic symptoms may not be prominent, or the presentation may be non-specific (4). This could be because of some physiological changes in the elderly that can alter the response to the disease, such as diminished pain perception, localization, and decreased thermoregulation (13). However, signs of peritonitis can be more pronounced (4). Atypical presentations of appendicitis in the elderly include vague symptoms such as nausea, vomiting, generalized abdominal pain, and decreased oral intake (14). Furthermore, they can present with changes in bowel habits in the form of diarrhea or constipation (15, 16). In addition, they can present with pain in atypical locations, such as left-sided abdominal pain or peri-umbilical abdominal pain radiating to the left side of the umbilicus (17, 18). Acute appendicitis in elderly patients is a challenging clinical entity, not only because of its challenging diagnosis, delayed presentation, and atypical clinical symptoms and signs, but also because it is associated with a higher rate of complications such as perforation, gangrene, and abscess formation (19). Exclusion of underlying malignancy is very important in this age group, especially cecal and appendicular tumors. Elderly patients with symptoms of acute appendicitis can harbor an underlying malignancy of the cecum or appendix, so it must be kept at the top of the differential diagnoses. As distinguishing appendicitis from colon cancer in elderly patients by symptoms or imaging may be challenging, a postoperative colonoscopy should be performed to exclude cancer (20). Moreover, they may have a delayed recovery with prolonged hospital stays due to their concomitant diseases and reduced physiological reserve. Underlying medical conditions, such as congestive heart failure and diabetes, can increase the risk of complications and affect the healing process. Moreover, elderly patients have reduced physiological reserve, which decreases their ability to withstand stress conditions such as surgical operations (21).

Abdominal ultrasound (US) is the first-line imaging choice in different populations (children, pregnant women). However, the overall sensitivity of 86% and specificity of 81% of US limit its usefulness in older populations (28). Acute appendicitis is not the most common pathological condition in elderly patients with acute abdominal pain, as it presents in 3% (28) to 5% (29) of all patients requiring computed tomography (CT). However, liberal use of CT is suggested in elderly patients with acute abdominal pain due to a broad spectrum of conditions, as it can influence the treatment plan in up to 65% of patients with positive CT findings, medical management in 52%, and surgical management in 48% (28). Unenhanced CT has been suggested for triaging elderly patients with acute abdominal pain (29). There are no data on sensitivity and specificity exclusively in the elderly, but in a meta-analysis in adult populations, the results of second-line US (sensitivity 83.9%, specificity 90.9%), CT (sensitivity 89.9%, specificity 93.6%), and MRI (sensitivity 89.9%, specificity 93.6%) are comparable and accurate (30). In a recent large randomized study comparing antibiotics with appendectomy (including patients with appendicolith), conservative treatment was proven non-inferior to appendectomy. After 90 days, appendectomy was performed in 29% of patients in the conservatively treated group (25% without appendicolith, 41% with appendicolith) (31). These data correspond to a long-term (5 years) follow-up of recurrence of appendicitis of 39.1% (32). In some of the recent meta-analyses from Germany and China, appendectomy still appears more effective as the definitive treatment, with different results regarding complications—fewer complications in conservative treatment were found in a Chinese meta-analysis, and no significant difference was reported in a German publication (33, 34). The incidence of acute appendicitis in the elderly is rising due to a longer life expectancy (36). This case report has been reported in line with the SCARE Criteria (44).
Conclusion
With increased life expectancy and the growing total population of elderly patients, there has been a rise in the number of cases of acute appendicitis in elderly people. Although acute appendicitis is not the most typical pathological condition in the elderly, it is not uncommon. Most of these patients require surgical treatment, and as with any acute surgical pathology in advanced age, treatment possibilities are affected by comorbidities, overall health status, and an increased risk of complications (22).
Acute appendicitis in the elderly constitutes a small percentage of total appendicitis cases, has a wide range of presentations, and is associated with a higher rate of complications, making it a challenging diagnosis. Thus, we believe that acute appendicitis in the elderly needs to be further studied and more data should be added to the literature, which will help establish the diagnosis of appendicitis to avoid delayed diagnosis and possible complications (6). Review shows that management of acute appendicitis in the elderly is not as straightforward as it is in the younger population. The elderly patient presents a diagnostic challenge regarding atypical presentations due to physiological changes with age, a wide variety of differential diagnoses, comorbidities, and their associated polypharmacy, and an appropriate choice of imaging modality. Although we are constantly striving for evidence-based treatment, available data on elderly patients with acute appendicitis are mainly retrospective and based on smaller groups of patients. Thus, the treatment plan should be based on each individual case as per the institution or the surgeon’s preference. Even in elective surgery, complications are more pronounced in the elderly population, and these are even more prominent in acute settings such as that of acute appendicitis (23).
Thus, we believe that acute appendicitis in the elderly needs to be further studied and more data should be added to the literature, which will help establish the diagnosis of appendicitis to avoid delayed diagnosis and possible complications (41). The non-operative management of uncomplicated appendicitis is a reasonable option in frail patients in order to avoid the burden of morbidity related to operation; nevertheless, surgery remains the standard of care in all age groups (42). Findings suggest an increased risk of peri-and postoperative complications among elderly subjects undergoing appendectomy, compared to non-elderly subjects (43).
Declarations
Ethical Approval and Consent to Participate
The content of this manuscript is in accordance with the Declaration of Helsinki for Ethics. No committee approval was required. Oral and written consent to participate was granted by her family.
Consent for Publication
“Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.”
Availability of Supporting Data
It is available.
Competing Interests
The author declares that they have no competing financial interests and nothing to disclose.
Funding: There is no funding.
Authors' Contributions
Ahmad Reza Shahraki is the surgeon of the patient and wrote this paper.
The author declares that they have no competing financial interests and nothing to disclose.
Acknowledgements
Acute appendicitis in the elderly constitutes a small percentage of total appendicitis cases, has a wide range of presentations, and is associated with a higher rate of complications, making it a challenging diagnosis. Thus, we believe that acute appendicitis in the elderly needs to be further studied and more data should be added to the literature, which will help establish the diagnosis of appendicitis to avoid delayed diagnosis and possible complications. The non-operative management of uncomplicated appendicitis is a reasonable option in frail patients in order to avoid the burden of morbidity related to operation; nevertheless, surgery remains the standard of care in all age groups. Findings suggest an increased risk of peri-and postoperative complications among elderly subjects undergoing appendectomy, compared to non-elderly subjects.
- Williams GR (1983). Presidential address: a history of appendicitis. With anecdotes illustrating its importance. Ann Surg. 197:495 506.
- Singh S, Bajorek B. (2014). Defining 'elderly' in clinical practice guidelines for pharmacotherapy. Pharm Pract (Granada) 12:489.
- Lander A. (2012). London: InTech Open. Appendicitis - A Collection of Essays from Around the World.
- Lapsa S, Ozolins A, Strumfa I, Gardovskis J. (2012). Geriatrics. Acute appendicitis in the elderly: a literature review on an increasingly frequent surgical problem. (Basel); 6:93.
- Peeters T, Houben B, Cools P. (2023). An observational study on lifestyle and environmental risk factors in patients with acute appendicitis. Heliyon. 9:0.
- Almusaylim MS, Foula MS, Al Amin JF, Al-Abbad MA, Alsaleh MA. (2024). Acute Appendicitis in an 86-Year-Old Patient: Uncommon Age for a Common Disease. Cureus.16(2):e54957.
- Martin RF. UpToDate. Philadelphia, PA: Wolters Kluwer; 2023. Acute appendicitis in adults: clinical manifestations and differential diagnosis.
- Su YJ, Lai YC, Chen CC. (2011). Atypical appendicitis in the elderly. Int J Gerontol. 5:117–119.
- Martin RF. UpToDate. Philadelphia, PA: Wolters Kluwer; 2023. Acute appendicitis in adults: diagnostic evaluation.
- Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. (2004). Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 141:537–546.
- Smink D. UpToDate. Philadelphia, PA: Wolters Kluwer. 2023. Management of acute appendicitis in adults.
- Park HC, Kim MJ, Lee BH. (2014). Antibiotic therapy for appendicitis in patients aged ≥80 years. Am J Med. 127:562-564.
- Pokharel N, Sapkota P, Kc B, Rimal S, Thapa S, Shakya R (2011). Acute appendicitis in elderly patients: a challenge for surgeons. Nepal Med Coll J. 13: 285–288.
- Williams N, Ronan O’Connell P, McCaskie AW. (2018). Bailey & Love's Short Practice of Surgery, 27th Edition. Boca Raton, FL: CRC Press. The vermiform appendix; p. 19.
- Deken MM, de Bie SH, de Noo ME. (2016). Acute appendicitis or colon cancer? The difference in elderly patients is not always clear. Ned Tijdschr Geneeskd. 160:0
- Asenjo-Alarcón JA, Vergara Cieza LE. (2023). Relationship between degree of dependency and hospitalization time of surgical patients. Invest Educ Enferm ;41:0.
- Sanda RB, Seliem SI, Omar E, Ashraf S. (2011). Perforated appendicitis in a septuagenarian. Ann Afr Med. 10:249–251.
- Ting JY, Farley R. J. (2008). Subhepatically located appendicitis due to adhesions: a case report. Med Case Rep. 2:339.
- Singla AA, Rajaratnam J, Singla AA, Wiltshire S, Kwik C, Smigelski M, Morgan MJ. (2015). Unusual presentation of left sided acute appendicitis in elderly male with asymptomatic midgut malrotation. Int J Surg Case Rep. 17:42–44.
- Ahn SR, Lee JH. (2021). Acute eosinophilic appendicitis: a rare cause of lower gastrointestinal hemorrhage. Korean J Gastroenterol. 78:134–137.
- Gaisinskaya P, VanHelmond T, Hernandez OL. (2022). Atypical appendicitis in the elderly. Cureus. 14:0.
- Lapsa S, Ozolins A, Strumfa I, Gardovskis J. (2021). Acute Appendicitis in the Elderly: A Literature Review on an Increasingly Frequent Surgical Problem. Geriatrics (Basel). 6(3):93.
- Ouchi Y., Rakugi H., Arai H., Akishita M., Ito H., Toba K., Kai I. (2017). Joint Committee of Japan Gerontological Society (JGLS) and Japan Geriatrics Society (JGS) on the definition and classification of the elderly Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr. Gerontol. Int. 17:1045–1047.
- Eskelinen M., Meklin J., Syrjänen K., Eskelinen M. (2021). A Diagnostic Score (DS) Is a Powerful Tool in Diagnosis of Acute Appendicitis in Elderly Patients With Acute Abdominal Pain. Anticancer Res. 41:1459–1469.
- Alvarado A. (1986). A practical score for the early diagnosis of acute appendicitis. Ann. Emerg. Med. 15:557–564.
- Chong C.F., Adi M.I.W., Thien A., Suyoi A., Mackie A.J., Tin A.S., Tripathi S., Jaman N.H., Tan K.K., Kok K.Y.Y. (2010). Development of the RIPASA score: A new appendicitis scoring system for the diagnosis of acute appendicitis. Singap. Med. J. 51:220–225.
- Lintula H., Kokki H., Pulkkinen J., Kettunen R., Gröhn O., Eskelinen M. (2010). Diagnostic score in acute appendicitis. Validation of a diagnostic score (Lintula score) for adults with suspected appendicitis. Langenbecks Arch. Für Chir. 395:495–500.
- Gardner C.S., Jaffe T.A., Nelson R.C. (2015). Impact of CT in elderly patients presenting to the emergency department with acute abdominal pain. Abdom. Imaging. 40:2877–2882.
- Barat M., Paisant A., Calame P., Purcell Y., Lagadec M., Curac S., Zappa M., Vilgrain V., Ronot M. (2019). Unenhanced CT for clinical triage of elderly patients presenting to the emergency department with acute abdominal pain. Diagn. Interv. Imaging. 100:709–719.
- Eng K.A., Abadeh A., Ligocki C., Lee Y.K., Moineddin R., Adams-Webber T., Schuh S., Doria A.S. (2018). Acute Appendicitis: A Meta-Analysis of the Diagnostic Accuracy of US, CT, and MRI as Second-Line Imaging Tests after an Initial US. Radiology. 288:717–727.
- CODA Collaborative A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N. Engl. J. Med. 2020;383:1907–1919.
- Salminen P., Tuominen R., Paajanen H., Rautio T., Nordström P., Aarnio M., Rantanen T., Hurme S., Mecklin J.-P., Sand J. (2018). Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 320:1259–1265.
- Yang Z., Sun F., Ai S., Wang J., Guan W., Liu S. (2019). Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 19:1–10.
- Prechal D., Damirov F., Grilli M., Ronellenfitsch U. (2019). Antibiotic therapy for acute uncomplicated appendicitis: A systematic review and meta-analysis. Int. J. Color. Dis. 34:963–971.
- Stewart B., Khanduri P., McCord C., Ohene-Yeboah M., Uranues S., Rivera F.V., Mock C. (2014). Global disease burden of conditions requiring emergency surgery. Br. J. Surg. 101: e9–e22.
- Ferris M., Quan S., Kaplan B.S., Molodecky N., Ball C.G., Chernoff G.W., Bhala N., Ghosh S., Dixon E., Ng S. (2017). The Global Incidence of Appendicitis. Ann. Surg. 266:237–241.
- Oeppen J., Vaupel J.W. (2002). Broken limits to life Expectancy. Sci. Compass. 296:1029–1031.
- Kraemer M., Franke C., Ohmann C., Yang Q., (2000). The Acute Abdominal Pain Study Group Acute appendicitis in late adulthood: Incidence, presentation, and outcome. Results of a prospective multicenter acute abdominal pain study and a review of the literature. Langenbeck’s Arch. Surg. 385:470–481.
- McGowan D., Howlader M., Patel R., Swindlehurst N., Manifold D., Shaikh I. (2011). Management and outcome of appendicitis among octogenarians in an English hospital over a five year period. Int. J. Surg. 9:669–671.
- Shchatsko A., Brown R., Reid T., Adams S., Alger A., Charles A. (2017). The Utility of the Alvarado Score in the Diagnosis of Acute Appendicitis in the Elderly. Am. Surg. 83:793–798.
- Shahraki A. R. (2024). Acute Appendicitis in a 95 Years Old male Patient:Uncommon Age for a Common Disease, A Case Report and Review of Literature.Chronicles of Clinical Reviews and Case Reports,The Geek Chronicles, 1, 1-8.
- Rondelli F, De Rosa M, Stella P, Boni M, Ceccarelli G, Balzarotti R, Polistena A, Sanguinetti A, Bugiantella W, Avenia N. (2019). Perforated vs. nonperforated acute appendicitis: evaluation of short-term surgical outcomes in an elderly population. Minerva Chir. 74(5):374-378.
- Yuan J, Chen Q, Hong W, Yu L, Li X. (2022). Comparison of Clinical Features and Outcomes of Appendectomy in Elderly vs. Non-Elderly: A Systematic Review and Meta-Analysis. Front Surg. 9:818347.
- Agha R.A., Franchi T., Sohrabi C., Mathew G. (2020). for the SCARE Group. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 84:226–230.
Download Provisional PDF Here
PDF



p (1).png)



.png)




.png)
